- Re: BMJ: Extra deaths not explained Archived Message
- BMJ: Extra deaths not explained - margo May 14, 2020, 2:09 pm
Posted by walter![]()
 on May 15, 2020, 12:04 pm, in reply to "BMJ: Extra deaths not explained"
on May 15, 2020, 12:04 pm, in reply to "BMJ: Extra deaths not explained"
|
Only one response in the BMJ so far to what, if true, is a grim development. Perhaps like me people are looking at the numbers hoping to find an explanation why it might not be as bad as painted; and, like me, not finding one. The ONS graph posted here (https://members5.boardhost.com/xxxxx/msg/1589284459.html): 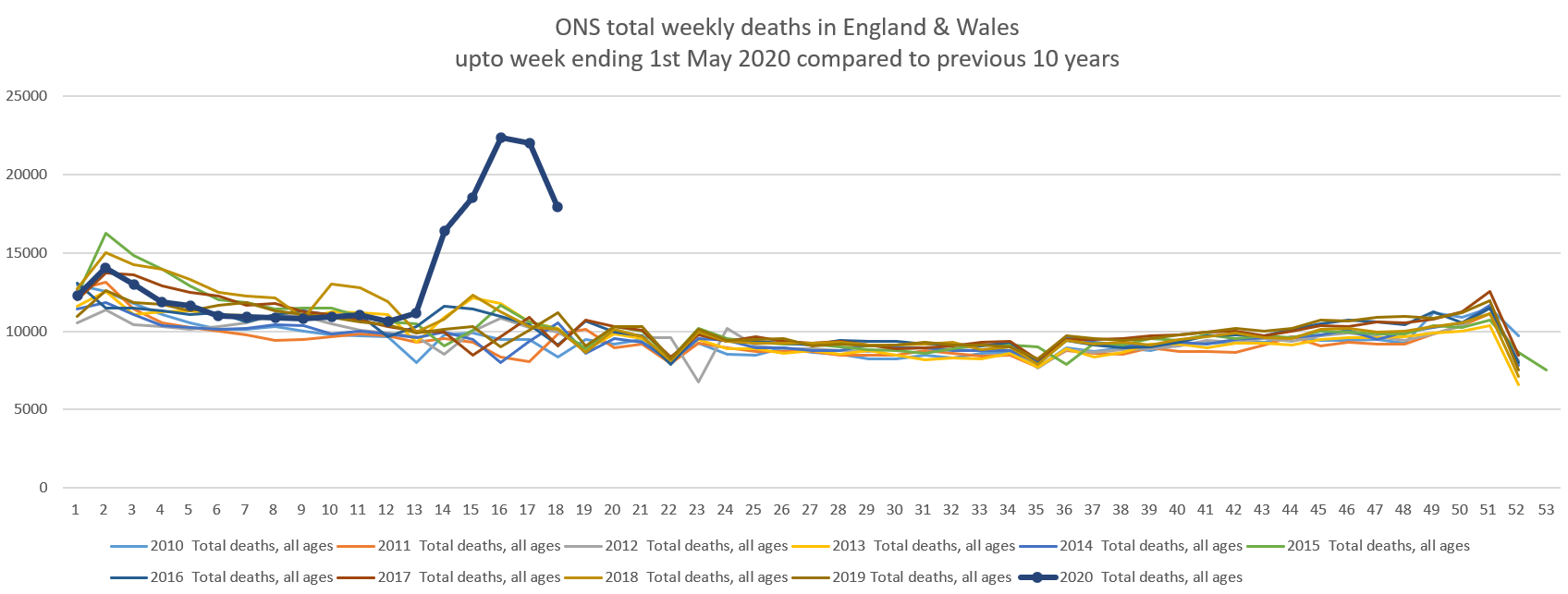 shows that over this 5-week period up to May 1st (see the five high points, ie the most recent ones) the numbers of deaths were around 16,500,18,500, 22,500, 22,000 and 18,000 respectively. Averaging about 19,500 deaths per week for those 5 weeks, as against a normal average for this period of 10,000 deaths per week. So, 9,500 extra deaths a week. 6,000 a week of these excess deaths are coming from care homes, it says (or 30000 over 5 weeks); that leaves only 3,500 excess deaths for the rest of the data, which includes the covid deaths, which in one week they put at 6000. Ah but once you remove the already-counted 2000 covid deaths a week that are in care homes, the numbers relate. It does seem that the mystery relates to the care home deaths and not the Covid-19 data. The one response in the BMJ: "Just to reflect that a while ago in discussion of this topic in the BMJ I recall a GP commenting on guidance being issued that made it less likely to include covid19 in causes of death in the absence of testing. He further commented along the lines of this made his completion of the paperwork far less onerous admin-wise. Think a key point to consider is that this Death certification is in the community, including care home settings where & when testing was unavailable. Given the significant extent & involvement of co-morbidities in the elderly vulnerable in particular, a GP can be in a place of some uncertainty when deciding cause of death in these circumstances." The BMJ claim seems to stack up with the ONS data and the guidance seems to support this. |
| Message Thread:
|